Case Report
It is not invisible! A case report of 2 patients with scalp Lichen Planopilaris mimicking Androgenic Alopecia

Sorbellini Elisabetta1, Pinto Daniela2, Marzani Barbara2 and Fabio Rinaldi1*
1Studio Rinaldi & Associati, Milan, Italy2International Hair Research Foundation (IHRF), Milan, Italy
*Address for Correspondence: Fabio Rinaldi, Studio Rinaldi & Associati, Milan, Italy, Tel.: +39-2-76006089; Email: [email protected]
Dates: Submitted: 24 November 2017; Approved: 06 December 2017; Published: 08 December 2017
How to cite this article: Sorbellini E, Pinto D, Marzani B, Rinaldi F. It is not invisible! A case report of 2 patients with scalp Lichen Planopilaris mimicking Androgenic Alopecia. Ann Dermatol Res. 2017; 1: 012-017. DOI: 10.29328/journal.adr.1001003
Copyright License: © 2017 Sorbellini E, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abbreviations: LP: Lichen Planus; LPP: Lichen Planopilaris; FFA: Frontal Fibrosing Alopecia; FAPD: Fibrosing Alopecia in a Pattern Distribution; VAS: Visual Analogue Scale; AGA: Androgenetic Alopecia
Abstract
Lichen Planopilaris is known as the form of Lichen Planus typical of the scalp. It is classified as a lymphatic disease and is characterized by chronic inflammation which leads to cicatricial alopecia. Its causes are not yet well characterized but its etiology seems to strongly correlates with infection, sensitization and pollution. A clear and objective diagnosis of Lichen Planopilaris is not simple but the evolution and strongly negative outcomes on scalp of people affected by, pose the need of an early diagnosis.
In this work we report the case of a 27-year-old male and a 54-year-old female, respectively, in which a correct diagnosis of Lichen Planopilaris, followed the incorrect previous ones, was made by means of dermatoscopy and histopathological analysis, decisive tools for the diagnosis of this kind of pathology.
Introduction
Lichen planopilaris (LPP), a morphological variant of Lichen Planus known as specific of the scalp, is a rare, difficult-to-treat, chronic, inflammatory skin condition resulting in cicatricial alopecia, which can be eventually permanent irreversible [1]. It has been described for the first time by Pringle in 1895 [2] and placed in the lymphocytic disease group by the North American Hair Research Society (NAHRS) [3]. The causes of this disease are not well clarified but it seems to act as an autoimmune disorder probably triggered by drugs, metal exposure, stress, pollution, contacts sensitizers or infection [4]. Epidemiological data report that about 0.5-1% of the population is affected by Lichen Planus and in particular, adult women result as the most affected population by LPP (ratio 1.8:1) [5,7], on people aged between 40-60 years and more frequently in Caucasian and Indian population than Asian ones [7,8] Its typical manifestation is multifocal areas of alopecia on the central scalp, usually accompanied by perifollicular erythema, hyperkeratosis, and subjective symptoms such as pruritus or pain [9]. Three different variants of LPP are normally recognized [3,9]: classic LPP, frontal fibrosing alopecia (FFA) [10] and Graham-Little Piccardi Lassueur Syndrome [11]. A fourth variant, known as fibrosing alopecia in a pattern distribution (FAPD) could be added if considering some cases of patients with androgenetic alopecia in which lesions identical to those seen in LPP were found [12].
The main therapy for LPP is topical treatment with class I or II, high-potency topical corticosteroids such as clobetasol propionate or intralesional triamcinolone injection [13]. Some other topical therapeutics approaches can include calcineurin inhibitors (cyclosporine, tacrolimus), even if limited data are reported. More recently also the use of mycophenolate mofetil has been proposed [13-16]. Driven by recent evidences on the role of peroxisome-proliferator-activated receptor (PPAR)-γ on the pathogenesis of LPP [17], also PPAR-γ antagonist, pioglitazone, has been recently included as effective therapy. In presence of severe not responsive cases, systemic and/or intralesional costicosteroids have been largely recommended [6] and tipically used in combination with topical corticosteroid treatment, with limitations as regards side-effects.
As typical when referring to scalp disease to make a clear and objective diagnosis is not easy. LPP manifestations evolve with the disease: early LPP can be easily confused with seborrheic dermatitis, on the other side, in the late stages, LPP can be confused with central centrifugal cicatricial alopecia (CCCA) and folliculitis decalvans [1]. The approach of differential diagnosis reveals to be crucial in order to counteract the progressive and chronic course of the pathology and to establish the correct therapy as well as the use of dermatoscopy and histological evaluation in condition in which LPP could result invisible at the clinical evaluation.
Case Report
Case report 1
A 27-year-old male (Milan, Italy), outdoor worker, reported a history of scalp thinning and hair loss for 1 year. Other symptoms reported were moderate pruritus, ≥4 according to VAS scale [18], erythema and scaling. No evidence of Lichen Planus in other body sites. All these symptoms were evaluated by the previous dermatologist as compliant with androgenetic alopecia associated with seborrheic dermatitis. Consequently, the patient was invited to treatment with Minoxidil 5% solution for three months. The therapy was then suspended because of erythema and itching worsening. Patient came to our examination because in his opinion hair loss and symptoms did not disappear. Physical examination of scalp confirmed erythema and localized thinning both in vertex and frontal area (Figure 1).
The area affected was also analyzed by a Dermatoscope with a 100x polarized magnification (Molemax HD, DermaInstrument, Vienna, Austria). The Molemax integrated software was used for images acquiring (Figure 2). Dermatoscopic examination confirmed the presence of erythema and scalp scaling mainly at perifollicular site but reported also the absence of significant miniaturization, which is typical of androgenetic alopecia. Dermatoscopy showed also the presence of tubular casts at the perifollicular level. Taking together the history of the patient and the latest evaluations, a preliminary diagnosis of LPP was made, subsequently confirmed by histopathological evaluation.
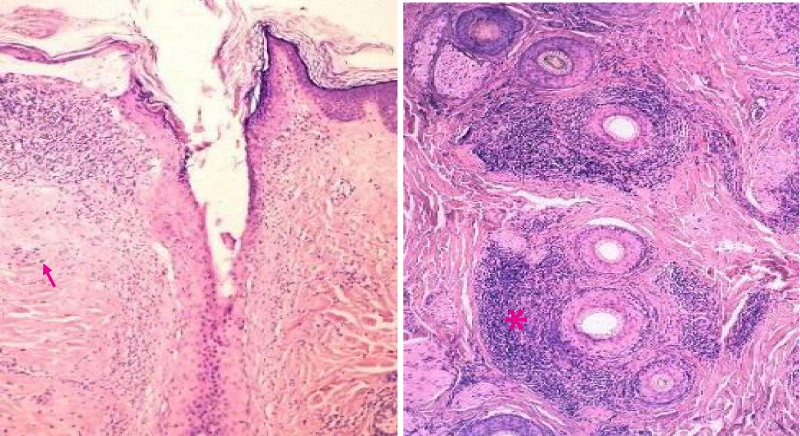
The analysis of histological section highlighted reduction in epidermis thickness, presence of skin sclerosis, vasodilatation, melanin pigment residues in the superficial dermis, vertical fibrotic bands and residues of pre-existing hair follicles (Figure 3). A dense peripheral lymphocytic infiltration was also found. All these observations were clearly consistent with LPP.
Figure 3: Histopathological analysis on case report 1, showing melanin incontinence on superficial dermis (red arrow), perifollicular infiltrates (asterisk).
Case report 2
A 54-year-old female came to our clinic reporting a history of therapy for telogen effluvium 2 years before. Patient went through menopause three years before and reported important symptoms such as sever osteoporosis, hot flush, insomnia, mood swings. Any hormone replacement therapy has been suggested to the patient because breast cancer familiarity.
Clinical evaluation showed scalp thinning both in vertex and frontal area (Figure 4). Patient referred also a persistent trichodinia. Also in this case no evidence of Lichen Planus in other body sites were found.
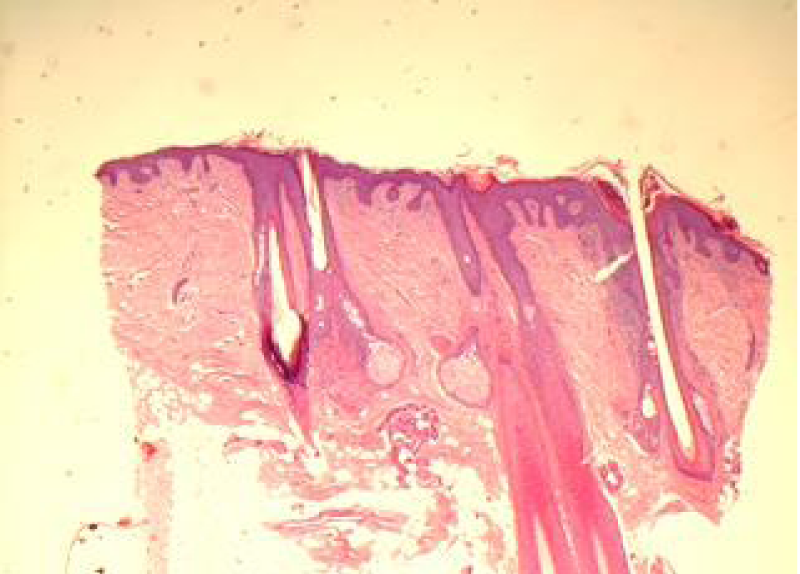
Patient anamnesis and clinical evaluation suggested the dermatologist to proceed further with dermatoscopic analysis. Images observation (Figure 5) revealed, among the rest, arborized vasodilatation, which is a typical manifestation of LPP. This diagnosis was finally confirmed by histology (Figure 6).
Treatment
After LPP diagnosis, both patients were treated with clobetasol propionate foam 0.05% on affected area once a day for 30 days, following by 15 days of resting and further 30 days of treatment once a day. Treatment succeeded into reduce inflammatory symptoms, also alleviating erythema, itching and fibrosis too. This contribute to stabilize LPP avoiding further evolution of the pathology as demonstrated by the following histopathological analysis.
Discussion
LPP is an uncommon scalp disease which diagnosis remains a challenge due to epidemiological data lacking and especially to the increasing number of patients in which lesions and symptoms are not clearly visible or evaluable if limited to patient clinical history and clinical observations. This led, in most cases, to a wrong diagnosis, preferably of androgenetic alopecia (AGA) with which LPP shares some macroscopic features. Some authors report these situations as “invisible LPP” [19,20]. The prognosis for LPP is worse than AGA, evolving into bulge stem cells disruption and scarring [6,21,22], leading to irreversible baldness. Therefore, LPP is often accompanied with persistent trichodynia, a burning scalp syndrome strongly affecting quality of life of patients, which are affected by [23]. From this the importance of an immediate and correct diagnosis for reducing LPP discomfort and stopping pathology evolution by early therapeutic intervention.
In the cases reported in the present work, we made a diagnosis of LPP, apparently invisible and following a previous wrong diagnosis, by means of dermatoscopic analysis coupled with histopathological examination. Patients were then submitted to treatment with clobetasol foam and this led the inflammation to be stabilized and at the same time hair loss stopping and trichodynia disappearance. Therapy with topical corticosteroid with mid-to high-potency is generally preferred as first-line the treatment of LPP with a resolution of the patology higher than 66% [5,6,23] confirming as the mainstay therapy for LPP.
According to our experience [24] LPP incidence is increasing with respect to reported statistics and this, probably, due to the impact on the pathology of etiological factors such as hair dying or microbioma dysbiosis [25]. There are also some studies demonstrating the involvement of environment in skin pathology including LPP [26, 27]. Pollution may act as oxidant agent and induce oxidative stress by increasing the production of reactive oxygen species (ROS) directly or indirectly [28]. LPP incidence is growing also because an improvement in diagnostic by means of dermatoscopy and histopathology that revel themselves as essential tools for make “visible” the “invisible”.
Informed consent
Written informed consent was obtained from the patient for the publication of this case report and accompanying images.
Conflict of interest
R.F. serves as a consultant for Giuliani S.p.A. P.D. and M.B. are employed by Giuliani S.p.A.
References
- Assouly, Philippe; Reygagne, Pascal. Lichen planopilaris: update on diagnosis and treatment. Semin Cutan Med Surg. 2009; 28: 3-10. Ref: https://goo.gl/hQEsUa
- Pringle JJ. Lichen pilaris spinulosus. Br J Dermatol. 1905; 17: 78-97.
- Olsen EA, Bergfeld WF, Cotsarelis G, Price V, Shapiro R, et al. Workshop on cicatricial alopecia. Summary of North American Hair Research Society (NAHRS)-sponsored workshop on cicatricial alopecia, Duke University Medical Center, February 10 and 11, 2001. J Am Acad Dermatol. 2003; 48:103-110. Ref: https://goo.gl/2xKT8p
- Cooper S. Lichen planopilaris. Orphanet. 2011; Ref: https://goo.gl/DhtZSB
- Chieregato C, Zini A, Barba A, Magnanini M, Rosina P. Lichen planopilaris: report of 30 cases and review of the literature. Int J Dermatol. 2003; 42: 342-345. Review. Ref: https://goo.gl/S2xHx1
- Nathaniel C. Cevasco, Wilma F. Bergfeld, Berna K. Remzi, Haydee Ramirez de Knott. A case-series of 29 patients with lichen planopilaris: the Cleveland Clinic Foundation experience on evaluation, diagnosis, and treatment. J Am Acad Dermatol. 2007; 57: 47-53. Ref: https://goo.gl/QBGnmV
- Hoon Kang, Abdullateef A. Alzolibani, Nina Otberg, Jeery Shapiro. Lichen planopilaris. Dermatol Ther. 2008; 21: 249-256. Ref: https://goo.gl/EfGFqh
- Lehman JS, Tollefson MM, Gibson LE. Lichen planus. Int J Dermatol. 2009; 48: 682-694. Ref: https://goo.gl/FH4R2u
- Weston G, Payette M. Update on lichen planus and its clinical variants. Int J Womens Dermatol. 2015; 16:140-149. Ref: https://goo.gl/3oMJ1N
- Samrao A, Chew AL, Price V. Frontal fibrosing alopecia: a clinical review of 36 patients. Br J Dermatol. 2010; 163: 1296-1300. Ref: https://goo.gl/ivZ831
- Odom RB, James WD, Berger TG, editors. Andrews’ Diseases of the skin. 9th ed. Philadelphia: WB Saunders Elsevier, Lichen planus and related Conditions; pp. 2006; 274-275. Ref: https://goo.gl/M8FbAp
- Zinkernagel MS, Trüeb RM. Fibrosing alopecia in a pattern distribution: Patterned lichen planopilaris or androgenetic alopecia with a lichenoid tissue reaction pattern? Arch Dermatol. 2000; 136: 205-211. Ref: https://goo.gl/WVnqba
- Whiting D. Cicatricial alopecia: clinico-pathological findings and treatment. Clin Dermatol. 2001; 19: 211-225. Ref: https://goo.gl/72CpDr
- Mehregan DA, Van Hale HM, Muller SA. Lichen planopilaris: clinical and pathologic study of forty-five patients. J Am Acad Dermatol. 1992; 27: 935-942. Ref: https://goo.gl/iPJsYo
- Tan E, Martinka M, Ball N, Shapiro J. Primary cicatricial alopecias: clinicopathology of 112 cases☆. J Am Acad Dermatol. 2004; 50: 25-32. Ref: https://goo.gl/CJ7igP
- Tursen U, Api H, Kaya T, Ikizoglu G. Treatment of lichen planopilaris with mycophenolate mofetil. Dermatol Online J. 2004; 10: 24. Ref: https://goo.gl/BC6BNF
- Mirmirani P, Karnik P. Lichen planopilaris treated with a peroxisome proliferator-activated receptor gamma agonist. Arch Dermatol. 2009; 145: 1363-1366. Ref: https://goo.gl/ft26KW
- Reich A, Heisig M, Phan NQ, Taneda K, Takamori K, et al. Visual analogue scale: evaluation of the instrument for the assessment of pruritus. Acta Derm Venereol. 2012; 92: 497-501. Ref: https://goo.gl/JGdR1s
- Nirmal B, George R, Kodiatte TA. Invisible lichen planopilaris unmasked by dermatoscopy. Int J Trichol. 2017; 9: 76-78. Ref: https://goo.gl/Gt1VVB
- Grupper MC, Buisson J, Durepaire R, Edelson Y. [Gougerot's invisible lichen planus]. Bull Soc Fr Dermatol Syphiligr. 1971; 78: 598-599. French. Ref: https://goo.gl/B5eGVt
- d'Ovidio R, Sgarra C, Conserva A, Angelotti UF, Erriquez R, Foti C. Alterated integrin expression in lichen planopilaris. Head Face Med. 2007; 3: 11. Ref: https://goo.gl/PZrmkS
- Baquerizo Nole KL, Nusbaum B, Pinto GM, Miteva M. Lichen Planopilaris in the Androgenetic Alopecia Area: A Pitfall for Hair Transplantation. Skin Appendage Disorders. 2015; 1: 49-53. Ref: https://goo.gl/f7BmaQ
- Chiang C, Sah D, Cho BK, Ochoa BE, Price VH. Hydroxychloroquine and lichen planopilaris: efficacy and introduction of Lichen Planopilaris Activity Index scoring system. J Am Acad Dermatol. 2010; 62: 387-392. Ref: https://goo.gl/opaHBT
- Sorbellini E, Pinto D, Marzani B, Rinaldi F. Considerations about Lichen Planopilaris and the correct diagnosis. JPD. 2017.
- He Y, Gong D, Shi C, Shao F, Shi J, at. Dysbiosis of oral buccal mucosa microbiota in patients with oral lichen planus. Oral Dis. 2017; 23: 674-682. Ref: https://goo.gl/Mqv6Fo
- Srivastava K. Urbanization and mental health. Ind Psychiatry J. 2009; 18:75-76. Ref: https://goo.gl/7grFsr
- Dlova N, Goh CL, Tosti A. Familial frontal fibrosing alopecia. Br J Dermatol. 2012; 168: 220-2. Ref: https://goo.gl/7grFsr
- Bickers DR, Athar M. Oxidative stress in the pathogenesis of skin disease. J Invest Dermatol. 2006; 126: 2565-2575. Ref: https://goo.gl/xXW3TJ