More Information
Submitted: May 01, 2021 | Approved: May 11, 2021 | Published: May 12, 2021
How to cite this article: Khallaayoune M, Mansouri S, Sialiti S, Hassam B. Follicular psoriasis: a poorly known presentation. Ann Dermatol Res. 2021; 5: 020-021.
DOI: 10.29328/journal.adr.1001017
Copyright License: © 2021 Khallaayoune M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Follicular lesions; Psoriasis; Spinulosis
Follicular psoriasis: a poorly known presentation
Khallaayoune M*, Mansouri S, Sialiti S and Hassam B
Department of Dermatology, Ibn Sina University Hospital, Mohammed V University, Rabat, Morocco
*Address for Correspondence: Khallaayoune M, Department of Dermatology, Ibn Sina University Hospital, Mohammed V University, Rabat B.P 6527 Morocco, Tel: (212)661509831; Email: [email protected]
Follicular psoriasis is an uncommon diagnosis and probably the least well-known subtype of psoriasis. Hence, we report the clinical and histological findings of follicular psoriasis in one patient to raise awareness of this rare entity.
Sir,
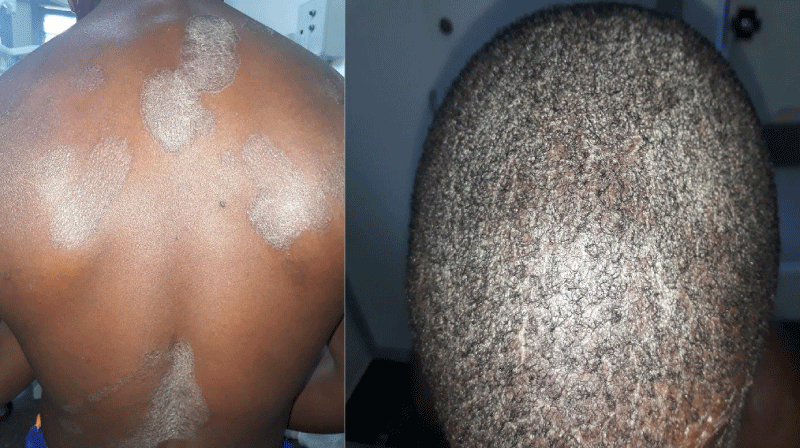
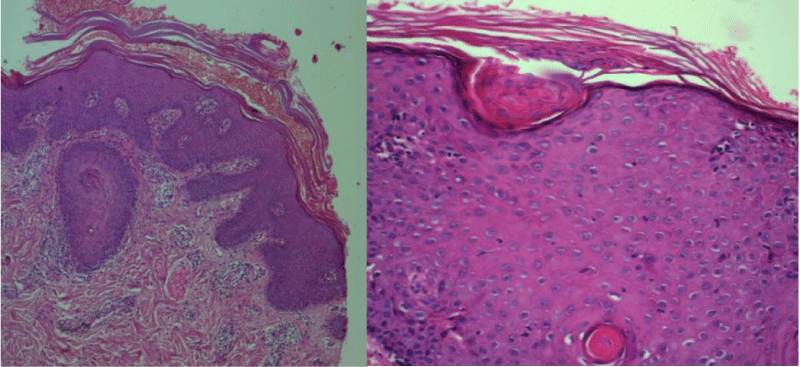
A 17-years-old young man presented with a one-year history of relapsing and remitting multiple asymptomatic-to-mildly itchy erythematous scaly plaques of different shapes and sizes. Anamnesis did not find any history of infection or prior drug intake. Clinical examination revealed multiple erythematous, spiny, 1–3 mm sized, follicular, hyperkeratotic papules resulting in plaques on the trunk, both elbows and knees, with diffuse scaly scalp (Figure 1). Scales were thin with a shiny appearance. Palms, soles and nails were not affected. General status was conserved and no lymphadenopathy was found. Histopathologic examination of a biopsy specimen taken from the trunk and arms showed acanthotis, hypogranulosis and marked parakeratosis in the follicular epithelium and the interfollicular epidermis with neutrophilic microabscess and keratotic plugs (Figure 2). Based on these findings a diagnosis of follicular psoriasis (FP) was made. Oral methotrexate was started allowing a remarkable clinical improvement. After eight weeks the patient was totally remitted and methotrexate was finally stopped after six months.
FP is an under-diagnosed variant among the other well documented forms of psoriasis with less than 30 cases described in the literature to date. It affects both sexes but in adults it may show a higher incidence in females [1]. It has been divided in two clinical subtypes: the adult form and the rarer juvenile form. The adult form is characterized by erythematous scaly follicular papules usually involving bilateral thighs, while the childhood form presents either as isolated plaques of confluent follicular lesions over the trunk, axillae, and bony prominences, or as a widespread eruption resembling pityriasis rubra pilaris (PRP). In the latest form follicular lesions may evolve into erythroderma [2]. FP may appear after years in patients affected by different subtypes of psoriasis, or, as occurred in our patient, previous history of psoriasis is not found and follicular lesions might present without classic features of plaque-type-psoriasis [3]. This last presentation is more frequent in children and could be an early stage of classic psoriasis as it may progress to other forms of the disease [3,4]. There seems to be a higher prevalence in dark-skinned patients and in those with plaque-type-psoriasis on the scalp [1]. An association with diabetes mellitus has also been reported [3].
Isolated follicular lesions may raise suspicion for several differential diagnoses, especially in juvenile patients where PRP might be difficult to distinguish from FP [4,5]. Histology shows follicular plugging dilatation and parakeratosis in both FP and PRP, but hypogranulosis and Munro microabscesses are not seen in PRP [4]. Other alternative diagnoses as lichen planopilaris, lichen spinulosus, follicular eczema, acute suppurative folliculitis or perforating dermatoses may be considered but are easily ruled out on the basis of specific clinical and histological findings of each condition.
In the literature, duration of the disease vary from 6 months to 23 years but a shorter evolution could be expected for young patients [6,7]. Prognosis and management does not differ from classic form. Treatment is based on conventional therapies of psoriasis as narrowband ultraviolet B light, or methotrexate [5,6]. Topical steroids are not documented in FP.
Figure 1: Plaques of follicular spin-sized scaly papules on the back with scaly scalp in a young black man.
Figure 2: Acanthosis, hypogranulosis and parakeratosis in the follicular epithelium and the interfollicular epidermis with neutrophilic microabscess and keratotic plugs.
- Stankler L, Ewen SW. Follicular psoriasis. Br J Dermatol. 1981; 104: 153-156. PubMed: https://pubmed.ncbi.nlm.nih.gov/7213548/
- Patil JD, Chaudhary SS, Rani N, Mishra AK. Follicular psoriasis causing erythroderma in a child: A rare presentation. Indian Dermatol Online J. 2014 J; 5: 63-65. PubMed: https://pubmed.ncbi.nlm.nih.gov/24616860/
- Nguyen CV, Farah RS, Maguiness SM, Miller DD. Follicular Psoriasis: Differentiation from Pityriasis Rubra Pilaris-An Illustrative Case and Review of the Literature. Pediatr Dermatol. 2017; 34: 65-68. PubMed: https://pubmed.ncbi.nlm.nih.gov/27874201/
- Babino G, Moscarella E, Longo C, Lallas A, Ferrara G, et al. Follicular psoriasis: an under-recognized condition. J Eur Acad Dermatol Venereol. 2016; 30: 1397-1399. PubMed: https://pubmed.ncbi.nlm.nih.gov/26289636/
- Ploysangam T, Mutasim DF. Follicular psoriasis: An under-reported entity. A report of five cases. Br J Dermatol. 1997; 137: 988–991. PubMed: https://pubmed.ncbi.nlm.nih.gov/9470921/
- Arps DP, Chow C, Lowe L, Chan MP. Follicular psoriasis. J Cut Pathol. 2013; 40: 859–862. PubMed: https://pubmed.ncbi.nlm.nih.gov/24074364/
- Thomas LJ, Dadzie OE, Francis N. Follicular psoriasis—a forgotten entity? Open Dermatol J. 2010; 4: 95–96.