More Information
Submitted: September 14, 2024 | Approved: September 19, 2024 | Published: September 20, 2024
How to cite this article: Alnabelsi S, Hasan R, Abdallah H, Qattini S. Non-surgical Treatment of Verrucous Hyperplasia on Amputation Stump: A Case Report and Literature Review. Ann Dermatol Res. 2024; 8(1): 015-017. Available from: https://dx.doi.org/10.29328/journal.adr.1001034 .
DOI: 10.29328/journal.adr.1001034
Copyright License: © 2024 Alnabelsi S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Prosthesis; Verrucous hyperplasia; Compression; Hygiene; Limb care
Non-surgical Treatment of Verrucous Hyperplasia on Amputation Stump: A Case Report and Literature Review
Sajeda Alnabelsi , Reem Hasan
, Reem Hasan , Hussein Abdallah
, Hussein Abdallah and Suzan Qattini
and Suzan Qattini
Department of Dermatology and Venereology, Damascus University, Damascus, Syria
*Address for Correspondence: Sajeda Alnabelsi, Department of Dermatology and Venereology, Damascus University, Damascus, Syria, Email: [email protected]; [email protected]
Verrucous hyperplasia is a wart-like lesion that can develop on amputation stumps, often due to poor-fitting prostheses, venous stasis, friction, and bacterial infections. While surgical excision is sometimes necessary for intractable cases, many instances can be managed non-surgically.
We present the case of a 35-year-old male with a slowly growing verrucous plaque on his amputated stump that had caused repeated infections. His prosthesis was loose, allowing the stump to hang loosely inside the socket. After histological confirmation of verrucous hyperplasia, he was advised to change his prosthesis and use compression bandaging. Over 5 months, the lesion resolved without surgery. Early recognition and non-surgical management, including proper prosthetic fit, compression, and hygiene, can often successfully treat verrucous hyperplasia of amputation stumps. This avoids the need for excision in many cases. Patients and clinicians should be aware of this condition and the importance of prosthetic fit and limb care to prevent and treat it.
An amputee’s residual limb especially in the lower limb is vulnerable to various dermatologic problems, such as contact dermatitis, callus, verrucous hyperplasia, ulcers, and cysts. Several factors contribute to the development of these problems. First, the skin is not physiologically adapted to tolerate the pressures applied to the residual limb by a prosthesis. Second, a fitted socket creates a closed environment where sweat is trapped and bacteria can proliferate. Finally, the materials of the prosthetic socket-limb interface may irritate or cause an allergic reaction to the underlying skin [1-3].
In this case report, we explore the clinical presentation, pathogenesis, and management strategies in general and for our patients especially.
We report a case of a 35-year-old unemployed smoker who has had a partial amputation of the lower limbs below the knee since he was six due to deformities and incomplete congenital development, after which he had to use prostheses to help him, which consisted of a supracondylar cuff, exoskeletal shank, and single axis foot. He had no other medical diseases that could cause the circulation problems.
The chief complaint started four years ago in the right lower limb in the form of asymptomatic well-defined plaques of ivory white warty papules some of them have a brownish tip.
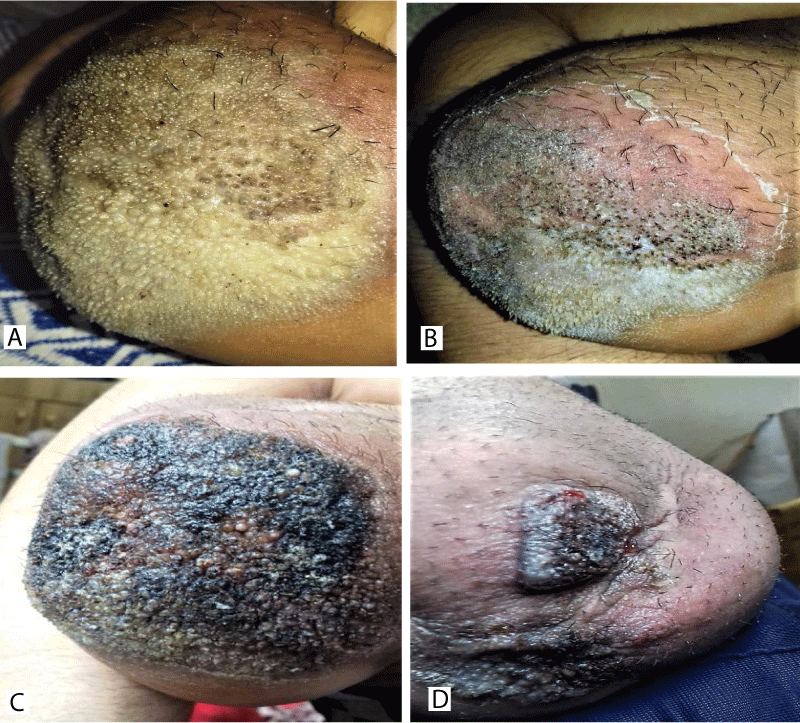
The lesion was treated as verruca vulgaris with topical keratolytic agents but without any improvement to be mentioned. Another smaller lesion on the left side developed two years after the right one began to form (Figure 1A-D).
Figure 1: Verrucous hyperplasia on amputation stump: the warty like lesions on the stump of the right lower limb (A), after treatment the lesions as verrucous vulgaris with topical keratolytic agents (B), the final appearance of the lesion when the patient visited our hospital (C), a similar small lesion developed on the stump of the left lower limb after two years of the right one beginning (D).
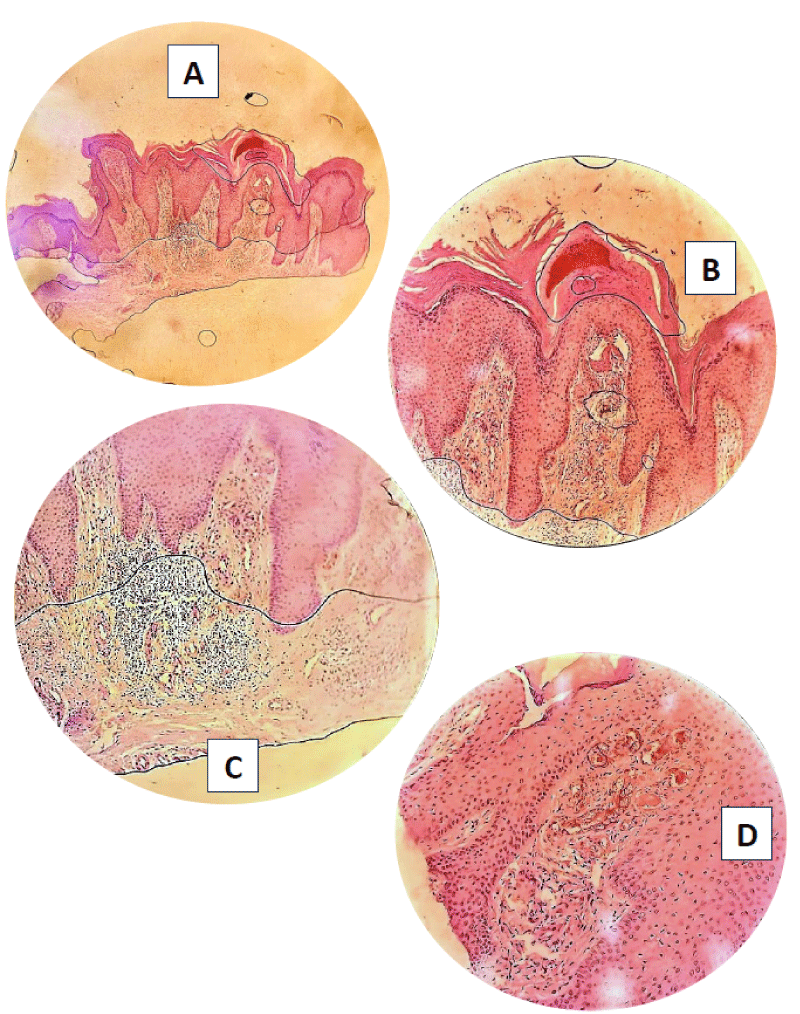
A skin biopsy was performed and showed nonspecific findings like papillomatosis, acanthosis, hyper and parakeratosis, proliferation and dilation in the blood vessels, mixed infiltration in the dermis, and the more specific lymphatic vessels dilation and proliferation (Figure 2).
Figure 2: Skin biopsy of the lesion: A. acanthosis, papillomatosis, hyperkeratosis in the epidermis (H&E, X 4). B. acanthosis, papillomatosis, hyper and parakeratosis in the epidermis (H&E, x 10). C. mixed infiltration in the dermis (H&E, x 40). D. proliferation and dilation in the blood vessels in the papillary dermis (H& E, x 40).
Based on clinical and histologic findings our diagnosis was verrucous hyperplasia in an amputation stump. The management was the replacement of the prosthesis with one consisting of a total contact socket, silicone sleeve suspension, aluminum shank, and single-axis foot, and using elastic bandage shrinker socks continually whenever the prostheses weren’t worn, with the possibility of letting the stumps free during sleeping.
In addition, topical antibiotics for 2 weeks to treat the bacterial infection. The patient was also instructed to daily carefully clean the skin using water and soap, and drying the skin completely. After 5 months of follow-up, all lesions disappeared (Figure 3).
Figure 3: The stumps of the lower limbs after 5 months of treatment : (A) the right side, (B) the left side.
Verrucous hyperplasia also known as papillomatosis cutis lymphostatica, lymphostatic congestion papillomatoses (e.g., elephantiasis), or papillomatosis cutis verrucosa (e.g., mossy foot) is a rare benign lesion that can arise on an amputation stump, with onset ranges from 6 months to 40 years after the amputation [4,5]. The first identification was reported by Ackerman, et al. in verrucous carcinoma in 1958 on oral mucosa, and this lesion was finally standardized as verrucous hyperplasia [6]. It presents as hyperkeratotic and papillomatous growth presents both diagnostic and therapeutic challenges and forms a unique clinicopathologic entity.
Key risk factors for developing verrucous hyperplasia on amputation stump have been implicated in the pathogenesis, including poor-fitting prosthesis, suction socket prosthesis, venous stasis, friction and chronic irritation, repetitive trauma, hygiene issues, and superimposed bacterial infections. These factors aggravate the main etiology which is the disturbance in the normal pattern of the vascular and lymphatic circulation, which in later stages causes a chronic edema, and subsequently verrucous hyperplasia, especially for those with transtibial residual limbs more than transfemoral [7].
Due to the clinical appearance of the lesions, many differential diagnoses can be considered such as Verrucous Vulgaris, tuberculosis verrucosa cutis, and verrucous Carcinoma [4,8,9].
Histologically, it shows pseudoepitheliomatous hyperplasia, dilated lymphatics and blood vessels, and mixed inflammatory infiltrate, without evidence of malignancy [4,8,9].
The management focuses on addressing the underlying causes rather than surgery. However, in some cases, surgical treatment could be an option if typical treatment fails.
The most effective treatments are:
Improving the fit and design of the prosthetic device to reduce chronic edema and friction. This involves using a properly fitted socket with adequate padding and suspension to minimize pressure on the distal stump [4,5,9]. Applying external compression, such as compression stockings or wraps, to address the underlying lymphedema. Maintaining good hygiene and skin care of the residual limb to prevent infection and further irritation [4,5].
In some cases, topical treatments like keratolytic agents and topical retinoids may help reduce hyperkeratosis. However, these treatments are often insufficient for extensive lesions. A short course of oral diuretics can be used if associated peripheral edema is present or an antibiotic if there is an infection [8].
The surgical approach options include: shave excision, and wide local excision, with flaps or grafts if necessary. Finally, CO2 laser ablation can be effective, particularly for recurrent or extensive lesions, offering precise removal with minimal damage to surrounding tissue [6].
Our patient presented with a warty, exophytic lesion on the amputation stump, which had progressively enlarged over time. The lesion was non-tender but cosmetically concerning and prone to minor trauma due to its protruding nature. The diagnosis of verrucous hyperplasia was confirmed through histopathological examination. Our management focused on the conservative side, including; changing the prosthesis and compression bandaging, and the lesion resolved over 5 months.
Verrucous hyperplasia on an amputation stump is an uncommon benign but potentially recurrent condition that requires a multifaceted approach to management. Accurate diagnosis through histopathological examination is essential to differentiate it from malignancy and other hyperkeratotic conditions. Treatment primarily involves conservative measures. Further research into the pathogenesis could improve preventative strategies and therapeutic outcomes for affected patients.
Ethical considerations
Informed, written consent was received from the patient for whom photographs are present in the manuscript.
- Meulenbelt HE, Geertzen JH, Dijkstra PU, Jonkman MF. Skin problems in lower limb amputees: an overview by case reports. J Eur Acad Dermatol Venereol. 2007;21(2):147-55. Available from: https://doi.org/10.1111/j.1468-3083.2006.01936.x
- Dudek NL, Marks MB, Marshall SC, Chardon JP. Dermatologic conditions associated with the use of a lower-extremity prosthesis. Arch Phys Med Rehabil. 2005;86(4):659-63. Available from: https://doi.org/10.1016/j.apmr.2004.09.003
- DesGroseilliers JP, DesJardins JP, Germain JP, Krol AL. Dermatologic problems in amputees. Can Med Assoc J. 1978 Mar 4;118(5):535-7. Available from: https://pubmed.ncbi.nlm.nih.gov/630514/
- George NM, George OT. Warty lesion over amputated stump. J Skin Stem Cell. 2021;8(2). Available from: https://brieflands.com/articles/jssc-119514
- Bardazzi F, Guareschi E, Savoia F, Varotti E. Verrucous hyperplasia in an amputation stump. G Ital Dermatol Venereol. 2003;138:499-501. Available from: https://www.minervamedica.it/en/journals/Ital-J-Dermatol-Venereol/article.php?cod=R23Y2003N06A0499
- Sharma P, Wadhwan V, Aggarwal P, Sharma A. Oral verrucous hyperplasia versus oral verrucous carcinoma: a clinicopathologic dilemma revisited using p53 as an immunohistochemical marker. J Oral Maxillofac Pathol. 2016 Sep-Dec;20(3):362-368. Available from: https://doi.org/10.4103/0973-029X.190902
- Grover S, Jha M, Sharma B, Kapoor S, Mittal K, Parakkat NK, et al. Verrucous hyperplasia: case report and differential diagnosis. Sultan Qaboos Univ Med J. 2017 Feb;17(1). Available from: https://doi.org/10.18295/squmj.2016.17.01.017
- Dhawan AK, Grover C, Bisherwal K, Arora VK, Tomar R. Verrucous hyperplasia of amputation stump. Indian J Dermatopathol Diagn Dermatol. 2015;2(1):23-24. Available from: https://journals.lww.com/ijdd/fulltext/2015/02010/verrucous_hyperplasia_of_amputation_stump.5.aspx
- Kim CW, Yang SY, Hahm JE, Kim KS, Ha JW, Kim SS. A case of verrucous hyperplasia of amputation stump. Program Book. 2018;70(1):458-459.