More Information
Submitted: January 23, 2025 | Approved: January 30, 2025 | Published: January 31, 2025
How to cite this article: Damiani L, Argenziano G, Ronchi A, Pagliuca F, Carraturo E, Piccolo V, et al. The Need of Wider and Deeper Skin Biopsy in Verrucous Carcinoma of the Sole. Ann Dermatol Res. 2025; 9(1): 005-007. Available from:
https://dx.doi.org/10.29328/journal.adr.1001036.
DOI: 10.29328/journal.adr.1001036
Copyright license: © 2025 Damiani L, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Carcinoma; Verrucous; Cutaneous; Foot; Cuniculatum; Biopsy; Diagnosis
The Need of Wider and Deeper Skin Biopsy in Verrucous Carcinoma of the Sole
Luca Damiani1* , Giuseppe Argenziano1, Andrea Ronchi2, Francesca Pagliuca2, Emma Carraturo2, Vincenzo Piccolo1 and Gabriella Brancaccio1
, Giuseppe Argenziano1, Andrea Ronchi2, Francesca Pagliuca2, Emma Carraturo2, Vincenzo Piccolo1 and Gabriella Brancaccio1
1Dermatology Unit, University of Campania “Luigi Vanvitelli”, Naples, Italy
2Pathology Unit, University of Campania "Luigi Vanvitelli", Naples, Italy
*Address for Correspondence: iLuca Damiani, MD, Dermatology Unit, University of Campania, Nuovo Policlinico (edificio 9C), Via Pansini 5, 80131, Naples, Italy, Email: [email protected]
Verrucous carcinoma is a rare, slow-growing squamous cell carcinoma that can occur in acral regions, including the plantar surface, being named carcinoma cuniculatum. The tumor presents as a well-demarcated, exudative lesion, resembling benign conditions like warts or infections. In this case, a verrucous lesion on the left plantar surface initially appeared to be non-malignant, with multiple incisional biopsies showing only inflammation. A final excisional biopsy of a large part of it confirmed the initial suspicion of malignancy, prompting complete excision and appropriate management. This case underscores the importance of performing wide and deep biopsies for early diagnosis and timely treatment of a suspected verrucous carcinoma.
Squamous Cell Carcinoma (SCC) is the second most common malignant skin cancer in the general population. The mean age at diagnosis is reportedly around 74 years of age in males and 77 years of age in females, with an incidence ratio M:F = 2:1 [1].
The main risk factors are fair skin phototypes and DNA repair deficiencies genodermatoses, along with natural or artificial ultraviolet radiation, ionizing radiation, chronic dermatitis and ulcers, human papillomavirus (HPV) infections, and chemical carcinogens skin exposition [1].
There are several SCC subtypes, including verrucous carcinoma. This uncommon SCC grows slowly and mainly in acral regions, being classified as carcinoma cuniculatum [1].
Further locations are the oral cavity (being named oral florid papillomatosis) and the anogenital region (giant condyloma of Buschke and Lowenstein) [2].
In the present paper, we report a case of verrucous carcinoma of the sole which required several biopsies, increasing in depth and wideness, to confirm the initial clinical suspicion.
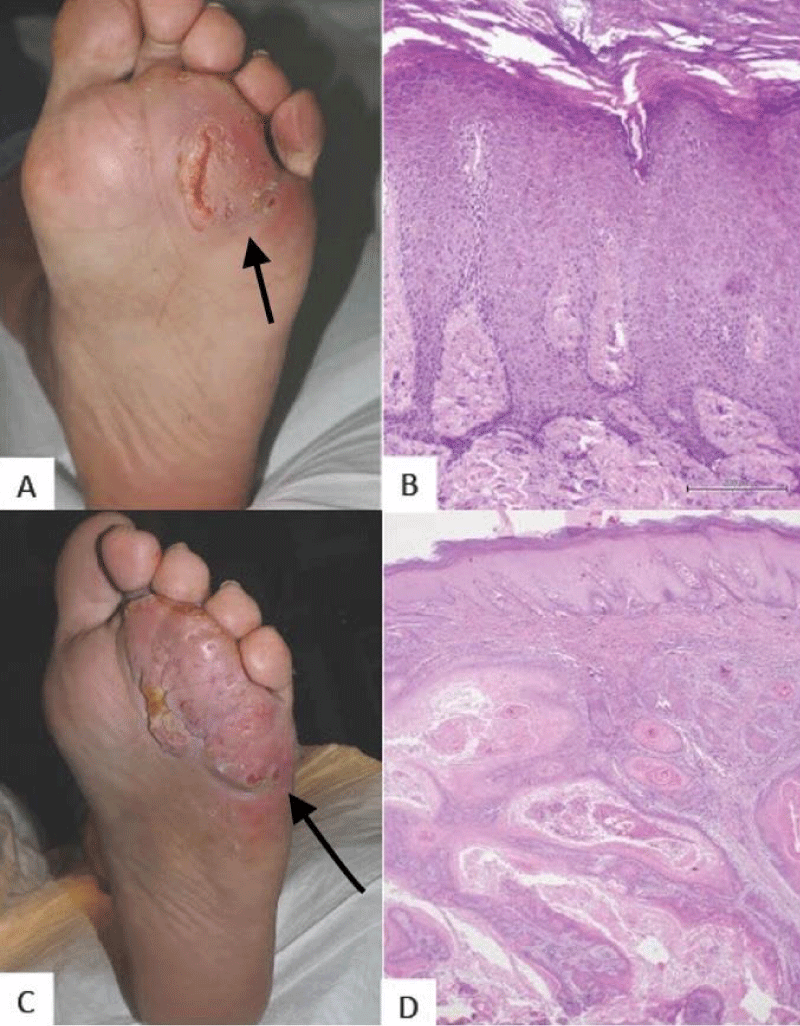
A 63-year-old diabetic male patient presented complaining of a verrucose, well-demarcated, skin-colored, exudating, painful plaque on the anterior region of the left plantar surface (Figure 1A).
The patient referred to its presence for more than a year, producing walking discomfort. He had previously taken minocycline and rifampicin oral therapy without benefit; and then performed a culture test positive for E. coli.
Clinical differential diagnoses included verrucous carcinoma, mycetoma, and atypical mycobacterial infection. We prescribed Trimethoprim/sulfamethoxazole oral therapy and planned a punch biopsy. Histological evaluation revealed markedly hyperplastic, acanthotic epidermis in the absence of significant keratinocyte atypia and the presence of focal spongiosis, moderate chronic inflammatory infiltrate of the dermis with eosinophilic granulocyte subsets (Figure 1B). Despite the absence of signs referable to malignancy, the clinical suspicion of skin cancer or an infectious lesion was still high.
A second incisional lozenge biopsy along with a deep swab was then performed, and excluded histological features of mycetoma and relevant keratinocyte atypia, showing again inflammation. Microbiology confirmed positivity for E. coli and Enterococcus faecalis.
Later, during a further evaluation, a new, more infiltrating component of the lesion was observed in the inferolateral area (Figure 1C). Given the relatively short time of growth and the clinical appearance, along with the poor response to antibiotic treatments, we decided to perform an excisional biopsy.
Histology revealed the presence of squamous proliferation in focal continuity with the epidermis, with endophytic growth in the dermis, consistent with a well-differentiated squamous cell carcinoma (Grade 1- G1) diagnosis (Figure 1D).
Figure 1: Plantar lesion at the first evaluation (A). Punch biopsy, hematoxylin and eosin stain: hyperplastic epidermis, with hyperkeratosis, acanthosis with no marked atypia of the keratinocytes, original magnification 100x (B). Plantar lesion at the last evaluation (C). Excisional biopsy, hematoxylin, and eosin stain: the squamous proliferation of the epidermis with dermis invasion, consistent with well-differentiated (G1) squamous cell carcinoma, original magnification 40x (D).
The case was then discussed in our multidisciplinary board; an MRI was prescribed to assess the degree of infiltration and a complete excision was scheduled in the Plastic Surgery department.
Histological analysis showed a well-differentiated squamous cell carcinoma (G1) of the left forefoot with excision margins free of malignancy.
Currently, the patient only performs annual dermatological examinations for skin cancer prevention.
Carcinoma cuniculatum is a verrucous skin carcinoma. It most commonly occurs on the anterior area of the plantar surface. It presents as an exophytic mass often misdiagnosed as a recalcitrant plantar wart [3]. Sometimes it presents multiple keratin-filled sinuses exuding smelling sebum. There typically is a long delay in diagnosis, given the clinical appearance resembling vulgar warts or other kinds of infectious lesions like mycetoma, and inflammatory conditions like reactive epidermal hyperplasia; other differential diagnoses include adnexal tumors, seborrheic keratoses, keratoacanthoma, verruciform xanthoma and verrucous melanoma [4].
Human Papillomavirus (HPV) types 6, 11, 16, and 18 have been found in various types of verrucous carcinoma, with HPV 6 and 11 being most commonly linked to those occurring in the anogenital region [5].
Histologically it is characterized by blunt papillary projections of well-differentiated epithelium (G1) with minimal atypia and surrounding inflammatory infiltrate. Tumor cells are large and pale staining with a benign appearance [6].
The tumor is locally aggressive initially compressing surrounding tissues and then destroying soft tissue and bone (around 10% of cases) [1]. Although local lymph nodes may be involved, metastatic spread is rare. The mortality rate is lower compared to other subtypes of verrucous carcinoma [7].
Treatment is wide local excision, up to partial or total foot amputation. In small tumors curettage and cautery may be effective [8,9]. Electrodesiccation, cryotherapy, and laser surgery show high rates of recurrence. It has been reported that photodynamic treatment and carbon dioxide (CO2) laser may be used to minimize tumor growth as neoadjuvant therapies [6]. Chemotherapy and radiotherapy have not been reported as treatment strategies.
Clinical diagnosis is often delayed because of the tricky appearance. Moreover, it frequently requires repeated incisional biopsies to achieve histological confirmation, the histology devoid of clear aspects of malignancy [10].
In the case we presented the first diagnostic suspicion was verrucous carcinoma but a diagnostic delay of more than six months happened because we relied on incisional biopsies.
In case of suspicion of verrucous carcinoma of the sole, a wider sample should be taken through deep shaving, excisional biopsy, or incisional biopsies by lozenge, in order to get the right diagnosis and ensure earlier and less invasive treatments.
Limitations and future perspectives
This case shows how performing a biopsy of a large specimen from the very beginning in the presence of a suspected cuniculatum carcinoma may allow earlier diagnosis and more effective and less invasive treatments. In the case of larger lesions, the risk of being non-diagnostic may remain, so more research is required about clinical and dermoscopic clues of malignancy in these tricky lesions to find the most suspicious areas to biopsy.
- Saurat JH, LD, TL. Dermatology and Sexually Transmitted Infection. 6th ed. Paris: Edra; 2018.
- Fawaz B, Vieira C, Decker A, Lawrence N. Surgical treatment of verrucous carcinoma: a review. J Dermatolog Treat. 2022;33(4):1811-1815. Available from: https://doi.org/10.1080/09546634.2021.1914312
- Nagarajan D, Chandrasekhar M, Jebakumar J, Menon KA. Verrucous carcinoma of foot at an unusual site: lessons to be learnt. South Asian J Cancer. 2017;6(2):63. Available from: https://doi.org/10.4103/2278-330x.208839
- Chauhan K, Jassal V, Sara GK, Bansal V, Hatwal V. Histopathological study of verrucous lesions and its mimics. J Microsc Ultrastruct. 2021;9(2):86-97. Available from: https://doi.org/10.4103/jmau.jmau_47_19
- Di Palma V, Stone JP, Schell A, Dawes JC. Mistaken diabetic ulcers: A case of bilateral foot verrucous carcinoma. Case Rep Dermatol Med. 2018;2018:4192657. Available from: https://doi.org/10.1155/2018/4192657
- Ye Q, Hu L, Jia M, Deng LJ, Fang S. Cutaneous verrucous carcinoma: a clinicopathological study of 21 cases with long-term clinical follow-up. Front Oncol. 2022;12:953932. Available from: https://doi.org/10.3389/fonc.2022.953932
- Farag AF, Abou-Alnour DA, Abu-Taleb NS. Oral carcinoma cuniculatum, an unacquainted variant of oral squamous cell carcinoma: a systematic review. Imaging Sci Dent. 2018;48(4):233-244. Available from: https://doi.org/10.5624/isd.2018.48.4.233
- Shwe Daniel S, Cox SV, Kraus CN, Elsensohn AN. Epithelioma cuniculatum (plantar verrucous carcinoma): a systematic review of treatment options. Cutis. 2023;111(2):E19-E24. Available from: https://doi.org/10.12788/cutis.0720
- Fawaz B, Vieira C, Decker A, Lawrence N. Surgical treatment of verrucous carcinoma: a review. J Dermatolog Treat. 2022;33(4):1811-1815. Available from: https://doi.org/10.1080/09546634.2021.1914312
- Nunes-Abreu F, Hidalgo-Caro R, Lorda-Barraguer E, Cristóbal-Redondo V, Céspedes-Guirao FJ. Consider carcinoma cuniculatum in recurrent foot ulcer: a case report and literature review. Arch Plast Surg. 2024;51(6):575-580. Available from: https://doi.org/10.1055/a-2316-3824